The Review Rate Fallacy: Why a 100% Review Rate Doesn’t Guarantee Improved Quality Metrics

As quality metrics and rankings continue to have an increasing prominence in the healthcare landscape, healthcare providers are looking for strategies to impact their quality metrics and ensure their data accurately reflects the care they’re delivering. One such strategy is pushing CDI departments to aim for a 100% review rate of cases, and while this goal may seem to have merit, the effort is misguided. Even if a CDI department was staffed to consistently reach a 100% review rate, this does not guarantee opportunity capture or improved quality metrics, and can, in fact, hurt CDI teams in the long run.
Shifting the Focus – Why Case Review Alone Falls Short of Maximizing Impact
While the common CDI metric of “review rate” can lead one to think that achieving a 100% review rate will result in improved documentation and complete opportunity capture, the reality is there is no inherent value in reviewing a case. There is no guarantee that a case review will result in a query, and so there is no intrinsic positive impact of a review alone, the true impact of a CDI department stems from queries. More accurate documentation, decreased likelihood of denials, more appropriate reimbursements are all results of queries. Putting undue focus on reviews (rather than queries) can also have negative downstream effects:
- CDI specialists can rush through reviews in order to meet a set volume of daily views, resulting in missed documentation opportunities
- Inconsistent querying practices driven by lack of attention to detail and process, can confuse providers, resulting in longer response times, and lower response and agree rates, contributing to additional documentation leakage
The end result of this pursuit is wasted time and misuse of precious clinical resources trying to review records with no documentation opportunity.
Strategic Work Allocation – Streamlining CDI Efforts in Times of Staffing Challenges
Inefficient workflows continue to be a problem that affects everyone in healthcare including clinicians facing burnout due to high administrative burden, and CDI departments facing staffing shortages. Automating non-clinical or administrative work is essential for healthcare organization survival¹.
Healthcare providers nationwide are facing staffing challenges, and CDI departments aren’t exempt from feeling the pinch, especially as nursing shortages continue to rise². With ever increasing staffing shortages it is vitally important to identify opportunities to automate workflows and minimize human toil on administrative tasks and operations. The Office of the National Coordinator for Health Information Technology (ONC) recently led a project to identify priorities that could accelerate health care workflow automation through the use of health IT and modern computing. One of the areas that could be greatly impacted by automation through technology was healthcare operations and more specifically, healthcare administrative workflows. An area considered “ripe” for automation was clinical documentation.
The purpose of a CDI program is to ensure that the clinical picture of the patient, the conditions being monitored and treated, are accurately reflected in the documentation and final codes. However, not every record has documentation opportunity. National surveys indicate that query rates are typically less than 30%, indicating that upwards of 70% records are reviewed unnecessarily. (ACDIS blog, 2018) With many CDI teams operating at historically low staffing levels, it becomes imperative to enable CDIS to work at top of license on the most impactful records, and reduce administrative toil – such as reviewing cases with no opportunity. To maximize documentation program resources, it becomes essential to identify the records with opportunity to minimize review effort on records without opportunity.
Still Relying on Traditional CDI? It’s Time for a Change
Old-school documentation tools are costing you revenue, rankings, and outcomes. Discover smarter ways to optimize documentation and outcomes.
AI/ML Revolution – How Technology Can Ease Case Review Burden
Clinical information can change daily (even hourly for some patients) therefore, on the surface, it is logical to plan to review every case every day to best capture documentation accuracy. However, doing so is not really effective as results or changes in patient status may come at a time later in the day meaning that the earlier review was for naught. Additional reviews when the documentation remains in alignment with the clinical picture also waste valuable time.
It is not necessary to have a human review each record every day as advances in technology can now solve this problem by identifying the records with the greatest likelihood of documentation opportunities. Rather than deploy expensive clinical resources to sift through records and comb through the data to identify documentation concerns, technology can review and automatically identify the records with a discrepancy between clinical evidence and documentation. This allows the clinical expert to have an automated list of records with the greatest statistical likelihood of a documentation opportunity that they can address and minimizes time spent in fruitless reviews.
When adopting ML-AI based prioritization as a methodology to create an effective worklist, different metrics should be utilized to track productivity and outcomes. Since the technology is reviewing every record in real time, it is no longer necessary to track the percent of all records reviewed. Instead it becomes important to review rates of prioritized records and the impact associated with reviewing those records. CDI workflow isn’t solely about reviewing records, it’s about compliantly impacting them, meaning creating meaningful change in the documentation that more accurately represents the clinical picture of the patient.
CDI at Work – Client Success Stories
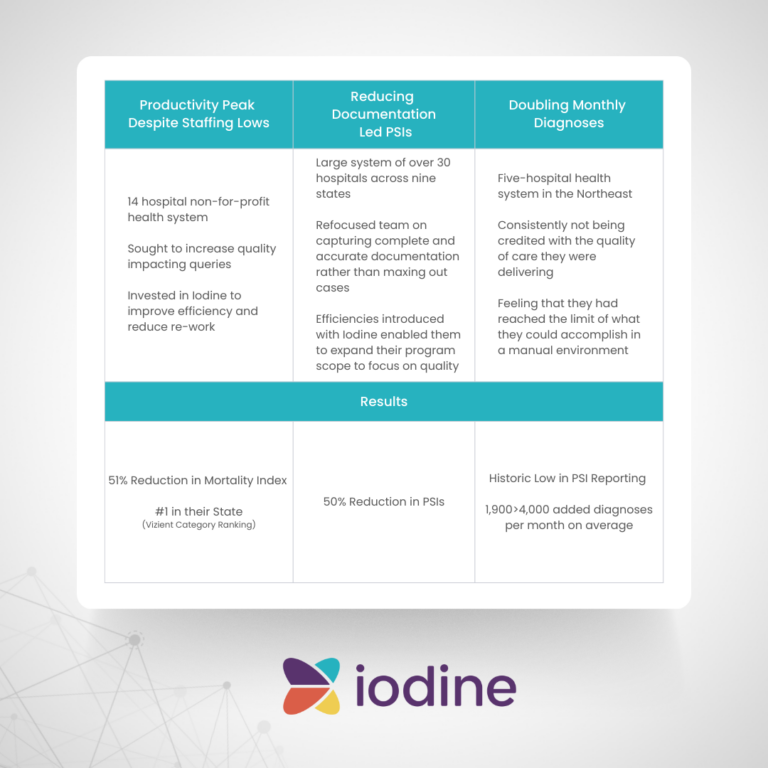
Not every record has documentation opportunity on a daily basis. Some may already have clear and consistent documentation of the conditions being monitored and treated. Others may not yet have enough clinical information to establish a working diagnosis. Reviewing these cases at the risk of missing others with documentation opportunity creates meaningless work with zero impact. Rather than focusing on reviewing every case, CDI staff should be held accountable for reviewing the cases that need a review, those with discrepancy between clinical evidence and provider documentation. This saves CDI staff countless hours attempting to review all records in hopes of stumbling upon documentation opportunities. Automating the creation of an ML-AI based prioritized worklist eliminates unnecessary reviews and increases the ability of the CDI team to focus on the records with likely opportunity. This results in capture of accurate and appropriate documentation and translates to capture of the patient’s full clinical picture and results in accurate reimbursement and reporting of quality metrics. (Iodine data graphic with results – here)
References:
¹Zayas-Cabán, Teresa, Saira Naim Haque, and Nicole Kemper. “Identifying opportunities for workflow automation in health care: lessons learned from other industries.” Applied Clinical Informatics 12.03 (2021): 686-697.
²Bouchrike, Imed. The U.S. Nursing Shortage: A State-by-State Breakdown in 2023. November 9, 2023
Still Relying on Traditional CDI? It’s Time for a Change
Old-school documentation tools are costing you revenue, rankings, and outcomes. Discover smarter ways to optimize documentation and outcomes.
Fran Jurcak is an accomplished senior executive with over 30 years of success in healthcare practice, education, consulting and technology. As a healthcare consultant, Fran leveraged her clinical and coding knowledge to support process improvement in the mid-revenue cycle, particularly in the clinical documentation integrity space. These process improvements allowed her clients to successfully minimize mid-cycle leakage and accurately report outcomes of care. She is currently the Chief Clinical Strategist at Iodine Software, where she has worked to bring artificial intelligence and machine learning technology to concurrent CDI workflow.
