Achieve Accurate, Reliable Reimbursement & Empower Your CDI Team
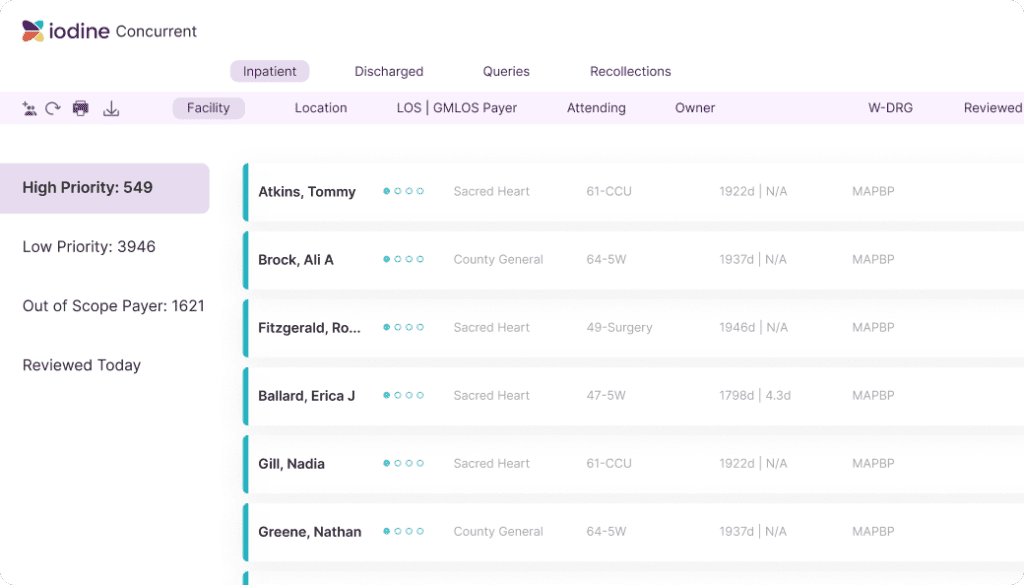
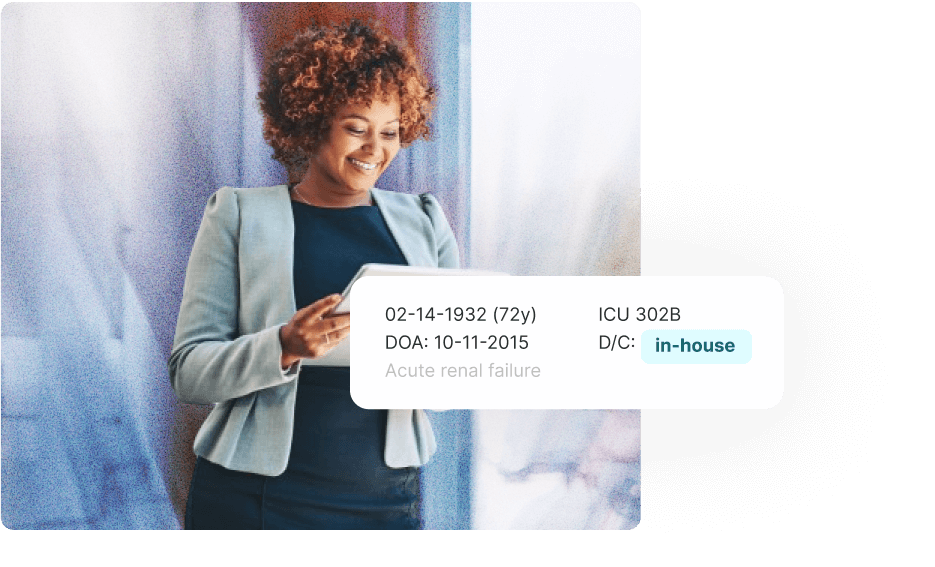
Iodine’s AwareCDI Suite harnesses cutting edge AI to drive consistent and accurate revenue capture, transforming CDI workflows. AwareCDI reduces manual workloads, prioritizing cases based on real-time data and financial impact, empowering CDI teams to achieve complete clinical documentation. This enables healthcare organizations to reliably maintain revenue integrity while upholding the highest standards of care, quality, and compliance.